

What’s in the Governor’s Budget for children’s mental health?
Highlights from the Governor’s Introduced Budget: 2020-2022
On December 17th, Governor Northam presented his proposed biennium budget to the Joint Money Committees of the General Assembly. His 2020-2022 proposed budget makes historic investments in key priority areas often overlooked—including behavioral health. Behavioral health priorities within his signature budget focus on the following: 1) children’s mental health initatives (woo hoo!), 2) Implementation of STEP-VA 3) Addressing high census at state psychiatric hospitals. Additionally, steps are taken to improve the behavioral health workforce challenges Virginia faces. These proposed investments total over $235 million in General Fund support to address the critical need in Virginia’s behavioral health system.
Virginia Mental Health Access Program (VMAP)
The proposed budget includes $4.2 million GF each year to complete statewide implementation of the Virginia Mental Health Access Program (VMAP). Beginning in 2019, VMAP is an integrated care pediatric program that increases access for children and adolescents to behavioral health services through enhanced pediatric training, psychiatric consultations, tele-health, and care navigation. Additional funding allows VMAP to be implemented statewide providing mental health training for primary care providers focusing on screening, diagnosis, management, treatment, referral and resources to address pediatric mental health disorders. In addition, three regional teams will be added to the existing two teams which provides two care navigators, one licensed clinical social worker, and one child psychiatrist for each region. Funding will allow for increased usage of the call center by providers seeking mental health resources for children, development of a database for care navigation system, as well as quality assurance and program evaluation of VMAP.
System Transformation, Excellence and Performance in Virginia (STEP-VA)
In 2017, the General Assembly expanded the core services of Community Service Boards (CSBs) to include same day access, primary care screening, crisis services, outpatient services, psychiatric rehabilitation services, peer support and family services, veteran support services, care coordination, and case management. These services are collectively called STEP-VA and must be fully implemented by June 30, 2021, according the code of Virginia.
Prior to STEP-VA, CSBs were statutorily required to provide only three services: emergency services, discharge assistance planning, and case management (subject to fund availability). As a result, all 40 CSBs provided the minimum three services but additional services, including children’s services, varied by locality. When fully implemented, STEP-VA will ensure consistency in core behavioral health services across the Commonwealth.
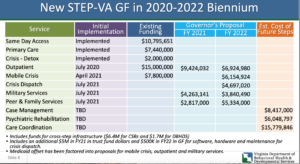
Building off progress and investments in STEP-VA since 2017, Governor Northam included $19.7 million in FY21 and $30.1 million in FY22 to buildout the following services: Outpatient mental health services for children and adults, Mobile crisis teams, Peer and family support services and veterans services. The proposal delays targeted case management for children and adults, care coordination and psychiatric rehabilitation until next biennium.
Additionally, $5 million NGF in FY21 and $500,000 NGF in FY22 from the DBHDS Trust Fund to improve the crisis response system. This funding will support the development of a maintain a statewide crisis hotline and startup fund for emergency dispatch.
Lastly, Funding was proposed to support administrative costs of STEP-VA, including 12 new positions that will aid in the implementation and management of STEP-VA; funds for training and certification of peer support services.
Fund implementation of Medicaid Behavioral Health Services
Provides $3 Million GF FY21 and $10.2 M GF FY22 and authority to establish and implement changes to services definitions, prior authorizations and utilization review criteria, provider qualifications and reimbursement rates for select Medicaid behavioral health services Specifically, multi-systemic therapy (MST) and family functional therapy (FST), residential crisis stabilization, intensive outpatient and 23-hour observation will be added as new Medicaid services. Medicaid rates will increase for the following programs: assertive community treatment (PACT), mobile crisis intervention, crisis stabilization, and partial hospitalization.
Behavioral Health Workforce Supports
Increase Mental Health Provider Rates. During the 2019 session, the General Assembly increased mental health provider rates to 100% of Medicare. Building off of this progress, Northam’s budget proposes increasing the psychiatric services rate by 14.7 percent. This action increases rates to the equivalent of 110 percent of the 2019 Medicare rates. This effort is critical because Medicaid reimbursement rates for mental health services has been historically low, contributing to providers refusing to accept Medicaid.
Behavioral Health Workforce Study and Training. $1 Million GF FY21 and $1.2 Million GF FY22 to conduct a behavioral health workforce study and train the behavioral heath workforce for upcoming changes in the behavioral health delivery system due to behavioral health redesign
Read More Blog Posts