

Nearly half of Virginia’s children are enrolled in Medicaid for their health insurance coverage. To ensure that these young people have access to mental health providers, and for those providers to adequately compensate staff, reimbursement rates for behavioral health must be increased this year.
Medicaid-funded services for children’s behavioral health has declined by $100 million since the beginning of the pandemic, largely due to the phase-out of Therapeutic Day Treatment Services in schools. While the dollar amount of funding has decreased, more children and youth have sought mental health services since the pandemic, meaning that services have not adequately kept pace with needs. Furthermore, only 14% of children on Medicaid are receiving behavioral health services, a significant gap below the need expressed in the general population of children and youth where 30% or more of young people express mental health concerns. Black and Latino children are disproportionately enrolled in Medicaid and report more barriers to accessing mental health care.
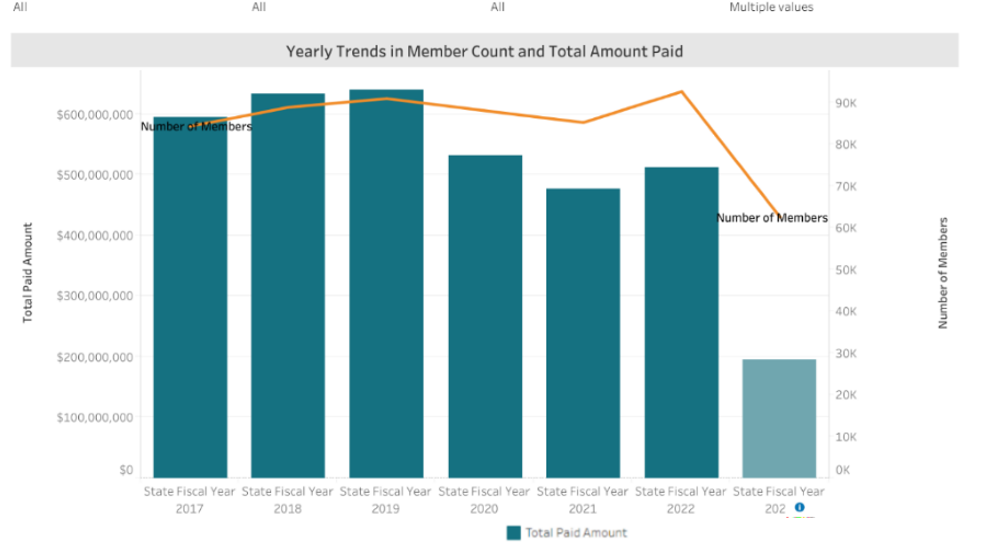
Medicaid reimbursement for children’s mental health services has declined by $100 million since the pandemic, despite an increase in children seeking services. (Bar on the far right does not represent a full year.)
The members of the General Assembly will consider several proposals to improve Medicaid reimbursement for behavioral health services. The options below can put Virginia on a path forward to bringing more behavioral health resources into schools and reaching more students who need mental health support.
Short-term solution: increase community behavioral health services rates in FY24
This proposal would provide:
And a long-term solution: conduct a rate study to determine inputs to delivering care and suggest a process for annual rate increases based on inflation.
Long-term solution: conduct a rate study on school-based mental health services to replace the currently offered service—therapeutic day treatment “TDT”. The future of behavioral health redesign planned to look at this service and develop new school-based services connected to multi-tiered systems of support in school.
This proposal provides a long-term solution to modernizing school-based mental health services and empowers young people to help design those services.
In a follow-up to the 2021 legislation proposed by Sen. Dunnavant to implement the “Free Care Rule” in Virginia, our state Medicaid agency has an application pending approval at the federal level to allow school divisions to bill Medicaid directly for school-based health and mental health services outside of a students’ IEP. This would enable school divisions to pull down a dollar-for-dollar match for the health services provided or initiated by schools. There is a catch though. School divisions will have to take on extra administrative tasks in order to seek reimbursement. This proposal allows DMAS to provide resources to DOE and school divisions to provide technical assistance and professional development to seek reimbursement.